Laura Z. Weldon, ND, MS is a naturopathic physician who loves exploring how people think, feel, sense, and connect. Weldon earned a doctorate in naturopathic medicine, a master’s degree in integrative mental health, an undergraduate degree in english literature and post-bacc pre-med degree. Her interdisciplinary research currently focuses on the pathophysiology and treatment of autistic burnout, and her work advocates for a neurodiversity paradigm shift across both medicine and society. She provides trauma-informed naturopathic consulting and coaching services, using herbs, nutrition, movement, health counseling, and craniosacral therapy to establish and embody a radical concept of wellness that includes autistic and disabled populations. This week she shared her research on autistic burnout and how she advocates for a neurodiversity paradigm shift in medicine.
When/how did you first realize you were autistic?
I was always fascinated by how people think, an early indication I was aware that something was different about my own internal process. I was 24 years old the first time a counselor suggested I may be on the spectrum, but it took another four years before I sought official diagnosis, and yet another year before I moved past my own internalized misconceptions about autism to fully accept it. Reading memoirs written by other autistic people, both speaking and non-speaking, and seeing my own experience reflected back to me made all the difference.
How did you first become interested in wellness and what does wellness mean to you?
I grew up doing pre-professional ballet which I loved, but it took a toll on my body. In college, I started doing Pilates as physical therapy and it opened my mind to the connection between form and function, how strengthening the feet could alleviate back pain, for example, and I became fascinated. Around this time I also started to show signs of chronic illness. Years of tests were inconclusive, and the improvement in my symptoms came as I gradually began to experiment with “alternative” medicine, removing food sensitivities, working with herbal medicine, and so forth. I was driven to understand how and why these approaches were so helpful and to share them with others, which led me to naturopathic medical school.
After nearly a decade working as a health coach and now as a naturopathic physician, I know first-hand the problematic issues in the “wellness community.” The wellness industry far too often puts forth an ideal of perfect health, often white, thin, fit, and self-reliant, that is unattainable and detrimental, disparaging difference and shaming most of our bodies and minds. Wellness should be accessible for us all: chronically ill, disabled, aging, neurodivergent, sensitive, mentally ill, Black and Brown, queer, trans, nonbinary, soft, sparkly, and matte ;-). There is no one right way to be well or take care of ourselves. What we each need to be able to answer “How are you?” with an honest “I’m well!” is unique, and my work is to help people redefine wellness in a way that is sustainable and fits with each individual’s experience and daily life. I celebrate the possibility of being autistic and well, disabled and well.
I am also part of the team at Autism Health and Wellbeing (Autism HWB), a website and online community where autistic people can share what they have discovered supports their own wellbeing. I love this site for two reasons particularly: one, it puts the power back in the hands of autistic people to define our own needs and supports, and two, it is all about community. Western concepts of wellness tend to be individualistic, all about “self-care,” but other cultures, including many of the indigenous N. American cultures I study, think about concepts of wellness in terms of community-care and connection. I see much greater potential for healing with a community-based approach, where autistic people can feel understood, accepted, included, and connected.
Your website says that one of its missions is to “advocate for a neurodiversity paradigm shift in medicine and society.” What does a neurodiversity paradigm shift in medicine look like?
A hope and a dream! Embracing a neurodiversity paradigm in medicine means accepting that all differences are not pathological, even when those differences may also be disabilities that deserve accommodation and support, such as autism. It means sorting autistic traits and differences from symptoms of autistic people in distress, and treating the underlying causes of that distress – not the difference itself. It means accepting different ways of playing, such as parallel play, as a neutral difference, while recognizing autistic burnout as a serious state of distress that warrants treatment. It means moving away from diagnostic overshadowing: far too often autistic people experiencing pain or severe anxiety have these symptoms lumped into “being autistic,” when they in no way need to be part of the general autistic experience. Perhaps most importantly, it means acknowledging that a lack of acceptance is the primary risk factor for autistic suicidality, so accepting these neurological differences is part of treatment and supporting the wellbeing of autistic people.
You also offer “trauma-informed naturopathic coaching and consultation.” What does that mean?
Providing trauma-informed care means acknowledging that trauma is pervasive, especially in certain communities (including the autistic community), and impacts mental, emotional, physical, and spiritual wellbeing. It means recognizing the signs and symptoms of trauma, including cPTSD, and integrating knowledge about trauma into policies, practices, and patient education. Trauma-informed providers are actively working to ensure people feel as safe as possible while receiving care. The principles of trauma-informed care are safety, choice, collaboration, trustworthiness, and empowerment.
Practically speaking, this means that my clients and I co-create the recommendations during each session and I write them up as experiments to try, rather than an official treatment plan, so if something doesn’t work with their life circumstances or they are unable to try it, they are not set up for failure and shame. With in-person clients, with whom I do craniosacral and other bodywork, it means everything is oriented around consent; I do not place my hands on someone unless their nervous system feels truly safe with me in that moment. It is also part of why I offer a 20-40% sliding scale option, no questions asked.
The difference between coaching and consultation is in the pacing. Consultations are full of information – they can be a second opinion, for a client who is self-directed but has specific questions for me, or for other professionals who want to discuss cases to better support their own patients. Coaching work is titrated; education is spread out over time, recommendations/experiments are paced so that they feel sustainable and integrated.
Can you explain some of the highlights or give a high-level summary of what you are currently researching related to the pathophysiology and treatment of autistic burnout?
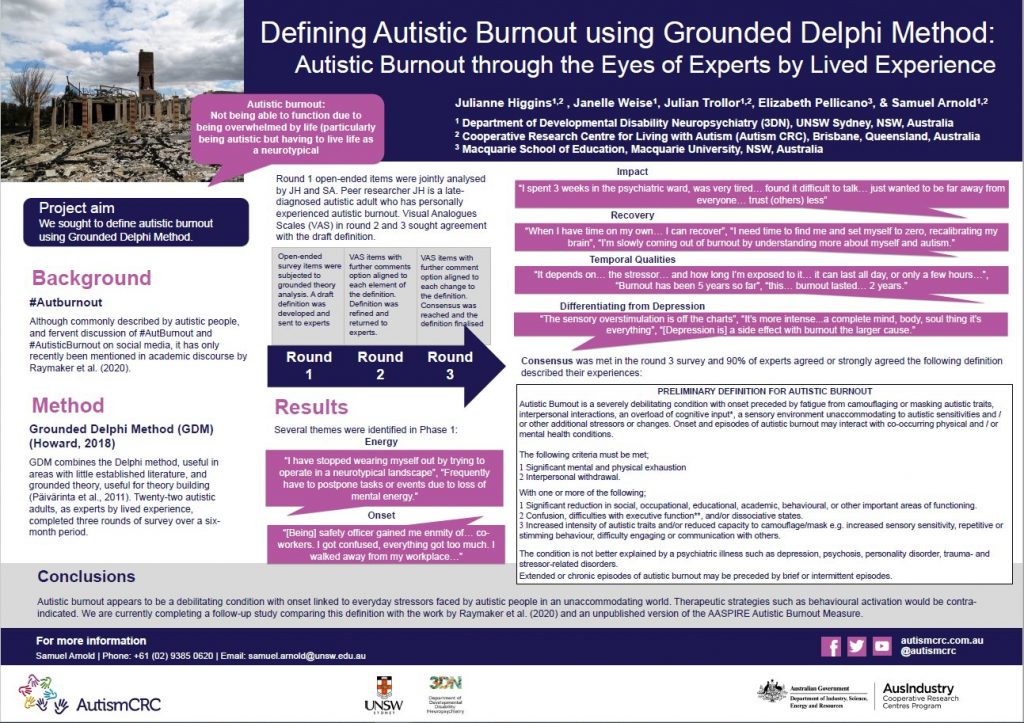
I think of autism as a neutral inherited neurotype with differences in cognitive, sensory, and social processing which increase an individual’s susceptibility to certain disorders, including autistic burnout, which I am investigating as a state of neuroinflammation. There are only two studies to date which seek to define autistic burnout and have determined it is distinct from other types of burnout, such as employee burnout, as well as depression. It is characterized by increased shutdowns, meltdowns, isolation, fatigue, sensory overload, and an exacerbation of conditions such as migraine and epilepsy. In childhood, it is referred to as autistic regression. The primary causes seem to be prolonged exposure to environments and demands not suited to autistic neurology (overstimulation, masking), as well as other co-occurring causes of neuroinflammation, including psychological trauma and traumatic brain injuries. As a naturopath, the best treatment is prevention, so much of this work is about understanding what contributes to autistic burnout and how to prevent or mitigate those factors (such as by advocating for autistic acceptance, which decreases rates of trauma). In terms of treatment, I work with a combination of lifestyle changes, external supports, nutrition, and herbal medicines that support and calm the nervous system.
You can access the full original study below, as well as the poster from the second published study on autistic burnout.
What are some of the most common wellness issues you see in your autistic clients and what kinds of support do you offer them?
The most prevalent theme in my work with autistic clients is a deep need for self-understanding and acceptance, as well as understanding and acceptance from others (including healthcare professionals). A lot of the support I offer is educational and seeks to validate experience, as well as “brain hacks” and ways to adjust our daily lives in the face of executive functioning challenges, autistic inertia, hyperfocus, and so forth. We focus on sorting difference from disorder – which aspects of our experience are things we want to accept and embrace, and which aspects cause us distress that we would like to shift.
Autistic people experience the same range of mental and physical health concerns as the general population, though there are more common patterns of presenting symptoms. I see a lot of people who have co-occurring hypermobile Ehlers Danlos syndrome, dysautonomia, and mast cell activation syndrome. Anxiety and insomnia are common and often associated with autistic burnout. For some autistic people, movement disorders such as apraxia seem to co-occur. Dissociation (disconnect from our bodies and/or environments) is also common and seems to be a result of both trauma and an adaptation to living in a world that is so constantly overloading/overwhelming. Digestive symptoms, headaches/migraines, seizure disorders, and autoimmunity also seem to be prevalent.
Is there anything else you’d like to say?
Thank you for your perspective, writing, and website. All parents of autistic children want the best possible lives for their loved ones, but I see such happier, healthier families when there is a basis of acceptance and support which so often comes from listening to and learning from autistic adults. Voices like yours bridge our communities in a beautiful and important way.
You can follow Weldon on Instagram @neurodivergentnaturopath.